In a follow-up on the malaria outbreak in Ethiopia, the surge in cases continues in the country.
According to the World Health Organization (WHO), between January 1 and August 18, 2024, 4,773,900 new malaria cases including 918 deaths were reported.
In spite of intensification of malaria response by the Ministry of Health, the cumulative number of malaria cases for 2024 so far already exceeds the total number of malaria cases for 2023.
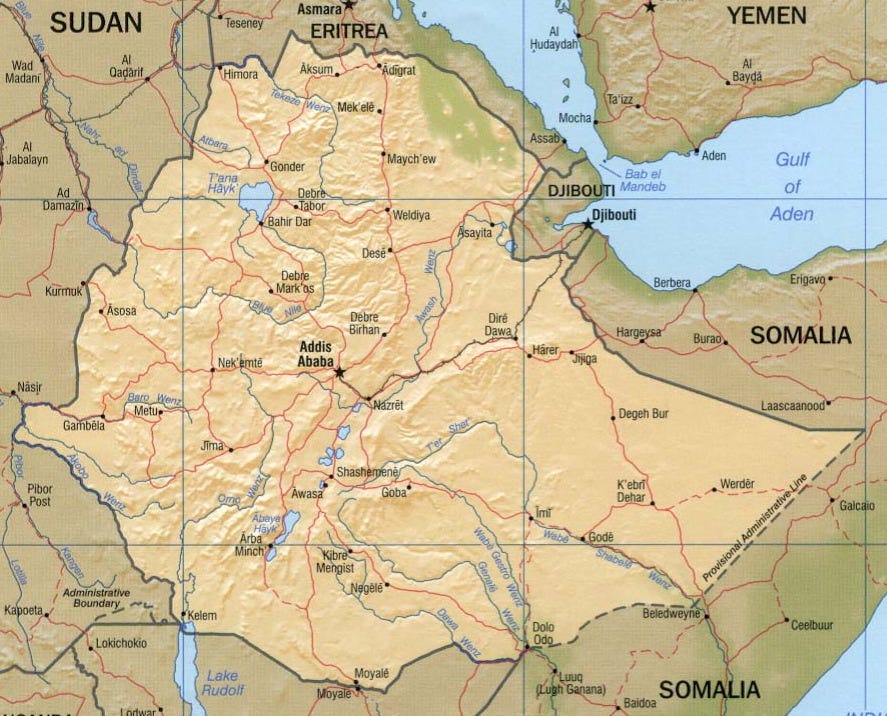
The majority of cases are reported from the following areas: Oromia (53%), Amhara (15%), Southwest (11%), South Ethiopia (5%), and Benishangul Gumuz (5%).
The highest number of cases per 100,000 population is reported from Southwest, followed by Benishangul Gumuz and Gambella.
Dr. Hiwot Solomon, Ethiopia MOH's lead executive officer for Disease Prevention and Control, stressed the severe impacts of malaria in sub-Saharan Africa, including Ethiopia.
Subscribe to Outbreak News TV on YouTube
She pointed out that 75% of Ethiopia's landmass is prone to malaria, affecting 69% of the population in those areas.
She stressed that malaria cases have risen over the past three years, necessitating urgent action.
Malaria is an acute febrile illness caused by a parasite known as Plasmodium. The disease is transmitted via the bites of infected mosquitoes. Of the four species that infect human beings, Plasmodium falciparum and Plasmodium vivax are the two most dominant malaria parasites in Ethiopia. They are prevalent in all malarious areas in the country (usually below 2000 meters above sea level) with P. falciparum representing about 65-75% of the total reported malaria cases, relative frequency varying in time and space within a given geographical ranges.
Symptoms of malaria include fever, headache, backache, joint pains, and vomiting, usually appearing between 10 and 15 days after the mosquito bite. If not treated, malaria can quickly become life-threatening by disrupting the blood supply to vital organs.
Key interventions to control malaria include: prompt diagnosis and effective treatment with appropriate antimalarial drugs, use of insecticidal bed nets; and indoor residual spraying of houses with insecticides to control the vector population.
However, the fight against malaria in Ethiopia faces significant challenges, including the emergence of insecticide resistance, changing weather patterns and severe weather events, and ongoing conflicts that disrupt malaria prevention and treatment campaigns.